Project Bo: Saving lives in Sierra Leone with Solar, Batteries and Twitter
In November 2017, browsing my Twitter timeline in the cab on the way to an industry dinner, I came across a Tweet that hit me like a punch in the guts:
“Three of our oxygen-dependent babies died last night when the power went off. Not good enough in 2017. Low-cost tech e.g. affordable solar power must be a priority for saving newborn lives.”
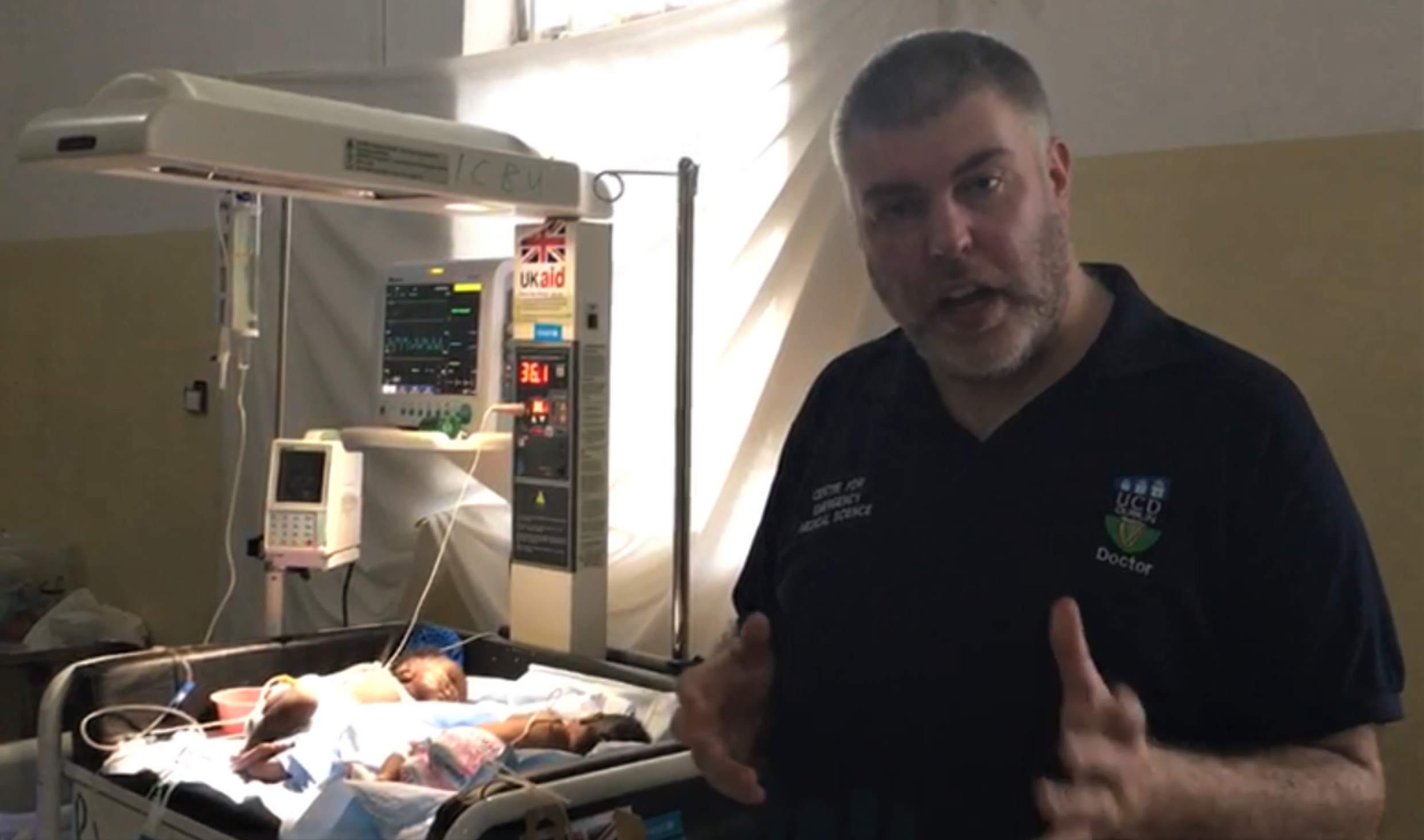
The Tweet was from Dr. Niall Conroy, Assistant Professor in Emergency Medical Science at University College Dublin, who had been shuttling between Ireland and Sierra Leone to set up a neonatal intensive care unit at the governmental hospital in Bo, the country’s third largest city, working with UNICEF and the Sierra Leone Ministry of Health and Sanitation.
Sierra Leone’s medical system was ravaged by the civil war which raged between 1991 and 2002. Then in 2014, the country was hit by Ebola, and for two years the country could focus only on mastering the outbreak, which claimed nearly 4,000 lives. In 2018, according to UNICEF data, Sierra Leone ranked second worst in the world for infant mortality, with 34 newborns dying for every thousand live births, and a further 48 dying before their fifth birthday.
For some context on the country’s energy landscape: In 2016, the World Bank reported that just over 20% of Sierra Leone’s population had access to electricity. Of that 20% with access, 46.9% live in urban areas, but only 2.5% live in the countryside. As of last year, the country’s 7.6 million population was served by just 170 MW of capacity. On average, Sierra Leoneans use just 61 kWh per person per year — just 1% of that used by the average EU resident, and 0.5% of the power used by the average American.
The neonatal unit at Bo Government Hospital is connected to the grid, but the grid is unreliable. The Bumbuna dam, completed in 2009 at a cost of $327 million, provides nearly half the country’s power. In the rainy season it delivers 50MW, but in the dry season the water level drops and it can manage only around 20MW, most of which is sent to the capital, Freetown. The rest of the country suffers frequent rolling power cuts, lasting as long as a week or more. Although there are plenty of plans and projects to increase generating capacity – including a $700 million 200 MW Phase II for Bumbuna, suppressed demand will easily mop up additional supply, and there is no chance that grid power in Sierra Leone is going to reach developed world levels of reliability in the foreseeable future.
From the point of view of a vulnerable baby in the neonatal unit at Bo Government Hospital, a 20 minute power cut can be tantamount to a death penalty. Infant-warmers, incubators and oxygen generators – which can be essential for survival – all require electricity: not huge amounts, but more than the average rooftop solar system serving just lights and phone chargers can supply, and it absolutely must be resilient.
It was hard to argue with the logic of Dr. Conroy’s tweet: It is indeed unacceptable that babies should be dying in this day and age because the local power supply is unreliable.
While others enjoyed the dinner, I reached out to Dr. Conroy. If he could handle the in-country side of things – permits from ministries, liaison with the hospital leadership – I committed to raising the money and managing the process of installing a reliable solar and battery system. I was lucky – because of my work with the UN’s Sustainable Energy for All initiative I could draw on a network of experts. Richenda Van Leeuwen, former Executive Director, Energy and Climate, Energy Access at the UN Foundation immediately volunteered to co-lead what we were soon calling Project Bo. My wife pitched in to build a website. Sonali Mehta and Harry Boyle, two early employees of New Energy Finance, now married, offered to help with fundraising. Laura Stachel, founder of We Care Solar, a US charity which provides solar systems for birth units in Africa, was a fount of advice.
We quickly settled on Energy for Opportunity, a Canadian NGO with operations in Freetown, as our local partner to design and build the system. Simon Willans, Executive Director and experienced African solar project developer, immediately sent a crew to Bo to scope the system. Within weeks we had the spec for a $100,000 system – 25 kW of solar PV panels and 125 kWh of battery storage – that would operate off-grid if necessary. We added in $5,000 to provide a tap so that the nurses no longer had to traverse the hospital lugging buckets of water, added a contingency of £25,000 for training, maintenance and unexpected costs, rounded the total to £100,000 and started fundraising.

The response was extraordinary. Within weeks we had raised the first $25,000, enough to order the batteries – the longest-lead-time item which had to be custom-built and shipped from the U.S. (we went for proven lead-gel Deka batteries rather than take a risk with lithium-ion). By the time they landed in Freetown, we had raised enough funds to build the whole system, and by August we had raised the full £100,000.
I am incredibly grateful for the generosity of our donors. A few were wealthy philanthropists; two institutions, the Hamburger Klimaschutz-Fonds (HKF) and Eurelectric (the association of European Electricity Utilities), were early supporters; but the majority were individuals who simply responded to our crowdfunding efforts – again mainly publicised via Twitter – and supported us with open hearts. I thank them all.
Project Bo’s system went live in September 2018. Once he has collected a year’s worth of comparable data, Dr. Conroy is planning to publish a peer-reviewed study of its impact. However, even based on preliminary data, it’s clear that it is saving lives. Controlling for other variables, it looks like mortality in the unit has dropped from 18% to 7% due to the advent of reliable power, potentially saving around eight lives per month.
If these figures hold up over time, the cost per life saved, assuming a system lifetime of just seven years, would be $156. This compares incredibly favourably with the oft-quoted record-low figure of $3,340 to save a child’s life via insecticide-treated mosquito nets. And there is no reason the Project Bo system should last only seven years – the batteries will need to be replaced around that time, but by then a new set should cost only $20,000 and will give another seven to 10 years of life-saving service.
We are still sitting on around $20,000 of the contingency raised as part of the appeal. The Project Bo steering group decided to spend it on initiatives that support maternal and neonatal health in Bo, rather than sit on it and wait until new batteries were needed. We donated $6,000 to We Care Solar for units at two maternal health units in the region around Bo, in recognition of their help. For the remainder, Dr. Conroy is working with the hospital leadership to identify the best use of funds, and will shortly submit a proposal. Most likely it will be spent on a dormitory for the mothers, who have nowhere to sleep while waiting to breastfeed babies admitted to the neonatal unit. Currently, they are sleeping outdoors and risking malaria, and in some cases, taking their babies home too early.
If it sounds like Project Bo was plain sailing, that is not entirely correct, there were certainly some rocky moments. And there were many lessons learned, which I believe are very much worth sharing.
First of all, here are five tips for anyone planning to undertake a project like Project Bo:
- Go for it! Project Bo has proven that solar and battery-powered mini-grids can save lives. As described above, we don’t yet have definitive data, but it is clear that the system is producing results. When Dr. Conroy visited the unit shortly after the system went live he asked the head nurse if the electricity was saving lives. Her response was unequivocal: “Yes, yes, yes. Less babies are dying now” (read more of Dr Conroy’s impressions of his first visit to Bo after the system went live here). Yes, Richenda Van Leeuwen and I had the benefit of existing contacts to help us complete Project Bo, but with some determined networking, anyone could have done it.

- Be ambitious but pragmatic. The first design Energy for Opportunity produced for the system was too small to run the equipment 24/7. The assumption was that right-sizing the system would make it too expensive. We insisted on a system that would solve the problem of intermittent power once and for all, and it was the right thing to do. However, we were also pragmatic: the system includes a small diesel generator, which can run the ward and charge the batteries in case of equipment failure. Given the choice between being 100% renewable or 100% resilient, when it comes to life-critical equipment, the choice is clear.
- Focus on governance. I refused to kick off fundraising for Project Bo until Dr Conroy talked me through the leadership structure at the hospital and reassured me that equipment and facilities could be secured from theft. Even so, when the system was first installed, three unapproved air conditioners were immediately and mysteriously connected to it, causing unexpected power outages with potentially fatal consequences. Only after emergency intervention from Energy for Opportunity and training of the nurses could we feel confident the system would not be abused.
- Budget for training and maintenance. This is something we insisted on from the start. We were determined to avoid the classic fate of the donor-funded mini-grid – it works fine when first installed, but no one is trained to use it, and there is no budget for maintenance. We set aside a contingency for regular visits by Energy for Opportunity to train the nurses and maintain the system, and financed a local store of spare parts (under lock and key). We are in the process of adding an internet connection so we can monitor system performance remotely.
- Plan for suppressed demand. Prior to the installation of the Project Bo power supply, the neonatal unit was admitting up to 70 patients per month. Over the past six months, admissions have been up to 110. In part, this may be due to the improved treatment on offer – it is too early to tell. Whatever the reason, we did not think hard enough about future demand growth when identifying system requirements and developing the engineering design. I would feel more comfortable had we raised $25,000 more and installed a bigger system.
Secondly, here are five messages for the NGO, multilateral agency, and donor community:
- Make medical appliances energy efficient. The equipment which drives demand for power at Bo Government Hospital’s neonatal unit – baby warmers, incubators, and oxygen concentrators – was donated by UNICEF at a cost of around $10,000 to $15,000. The Project Bo power system we built cost up to 10 times as much as the equipment it supplies! As things stand, there are no more efficient models on the market than the ones in use in Bo. But I am willing to bet that with a bottom-up redesign, their power demand could be halved. Even if the equipment cost were to double (which I sincerely doubt), the overall cost to provide life-saving care would be reduced. Come on medical equipment suppliers, let’s have models designed around the realities of the power supply in the developing world!
- Reduce mini-grid system costs. Although the cost per life saved by Project Bo looks set to be incredibly low, $100,000 is a huge amount of money for a single hospital ward’s power supply, in the context of a country where GDP per capita is just $510. There is a need for resilient power throughout the health system in the developing world, but there will not be many other use cases where so many lives can be saved with such a simple intervention as in an urban neonatal intensive care unit. By standardising designs and procuring in bulk, it should be possible to reduce the cost of this type of resilient power supply, so they can be deployed throughout developing country health systems.
- Create a clear customs waiver programme. The biggest uncertainty we experienced in budgeting for Project Bo was whether or not our equipment would be subject to customs duties. In general, humanitarian supplies are given a waiver, but you can’t bank on it up front. To receive our waiver, Energy for Opportunity and the hospital to request it from the Health Ministry, who had to inform the Finance Ministry, who had to inform Customs and Excise. None of this could be initiated until we had a Bill of Lading, which means precious time was lost. The multilateral community must surely be able to set up a robust pre-approval process, or even a blanket waiver of customs duties on clean energy equipment, given how vital it is for health, education, and economic development.
- Proactively capture health-related power data. All we knew when we started Project Bo was that babies were dying because of power cuts. We had no idea how frequent they were, or how long they lasted. To this day, I have no idea if this data exists for Sierra Leone, the city of Bo or the hospital. As a result, we had to design a system that could effectively operate off-grid. With a year’s worth of accurate data, we might have been able to design a cheaper system – one with a smaller battery, or perhaps even one with no solar panels, using just intermittent grid power. In the case of Project Bo, the humanitarian need was so pressing, we did not have the luxury of collecting data before designing the system. A massive data-logging exercise focused on power quality at health facilities in developing countries would be a very good use of aid money.
- Get smart about energy and aid. Let me be blunt: there is little point donating baby warmers and oxygen concentrators to a neonatal unit if the power supply is intermittent. I don’t want to be too harsh on UNICEF because they are far from the exception: the developing world is full of donor-funded equipment, at best run from diesel generators with horrible environmental impacts and unacceptable power quality, and at worst sitting unused until it disappears. Donors and aid agencies need to think of the power supply as an integral part of their offering, whether in health, education, agriculture, or economic development; they need to work shoulder-to-shoulder with the best clean energy NGOs, and everyone must be measured by the same metrics.
In summary, Project Bo has demonstrated beyond a shadow of a doubt that clean energy can help make dramatic, rapid improvements in health outcomes among some of the most vulnerable populations in the world. However, these improvements will not accrue automatically through generic improvements in energy access. In health care, power quality – especially reliability – matters as much as quantity.
We need to take the lessons from Project Bo and from an increasing number of other projects like it, and apply them at a programmatic scale. There may be no other single intervention that could deliver such substantial improvements in health outcomes for vulnerable patients in poorer developing countries.
Finally, Project Bo was one of the most humbling and gratifying initiatives I have ever led. I can only thank our donors, Richenda Van Leeuwen and the other members of the Project Bo steering group, and the ever-inspiring, selfless Dr. Niall Conroy, whose tweet back in November 2017 was the catalyst that launched Project Bo.